Reducing disparate outcomes with digital health tools
2 Dec 2022 07:45h - 08:45h
Event report
During the COVID-19 pandemic, the uptake of digital health services was consequently increasing. This uptake was propelled both by the necessity of the circumstances and by special allowances, such as the declaration of a public health emergency in the USA, setting aside legal restrictions preventing the uptake and use of different digital health modalities. With the pandemic threat receding, the use of digital health tools has dropped from the height of pandemic level, but is still above the pre-pandemic level. The discussion in this session builds on the two years of experience in charting a way forward for the future of digital health.
The development of digital health care creates a level playing field for many people who remain unserved by the physical health system. From patients in rural areas to those with rare and complicated diseases, it enables patients to find health care when doctors and hospitals are unavailable nearby. It is more convenient and helps to save commute time and hospital waiting periods. It allows continuity of care by enabling patients to see the same provider in case patients or doctors move elsewhere. It also provides health data interoperability, preventing time loss in emergency cases when patient records can expedite diagnosis.
It was stated that digital health care is a massive win for mental health-related issues in particular. Research proves that qualities of service between online and in-person psychotherapy are comparable. Online psychotherapy allows an additional advantage of anonymity as patients do not have to go to a building to visit a doctor. It even enables people in suburban and rural areas to access mental health services.
However, numerous challenges plague the health care movement from in-person to online. Access is compromised because of infrastructure-related deficiencies like patchy internet access and lack of electricity in remote places. Concerns regarding the privacy and safety of patient confidential data need addressing to mitigate the risk of informational harm. Quality of care is not comparable to advanced procedures and surgical intervention. Legal restrictions complicate the matter further as regulation and clarity on many issues are needed, most notably on health insurance claims.
With the spike in the number of digital health care providers and digital well-being apps, challenges abound because not all tools and services are of uniform quality. These are rarely evaluated for effectiveness and trustworthiness. Thus, an effort is needed to institutionalise digital health in the existing health system. Access to the internet and tools that people need for health care should be made available. Providing suitable cybersecurity measures in health care settings can help resolve safety and privacy concerns. Ensuring special provisions can ensure accessibility for people with disabilities. Finally, promoting digital health literacy so that people can meaningfully participate is still necessary.
By Kaarika Das
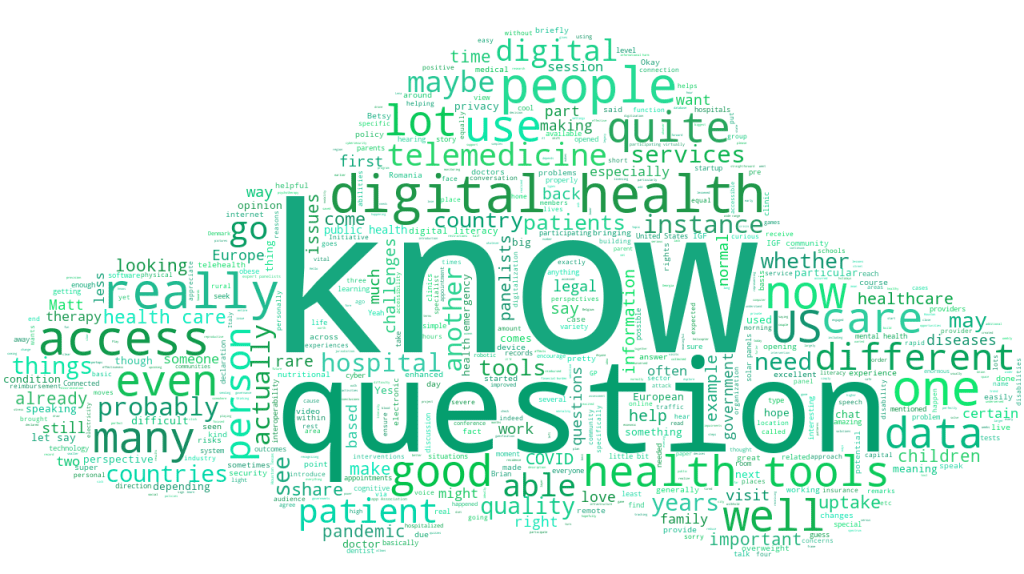
The session in keywords
Related topics
Related event